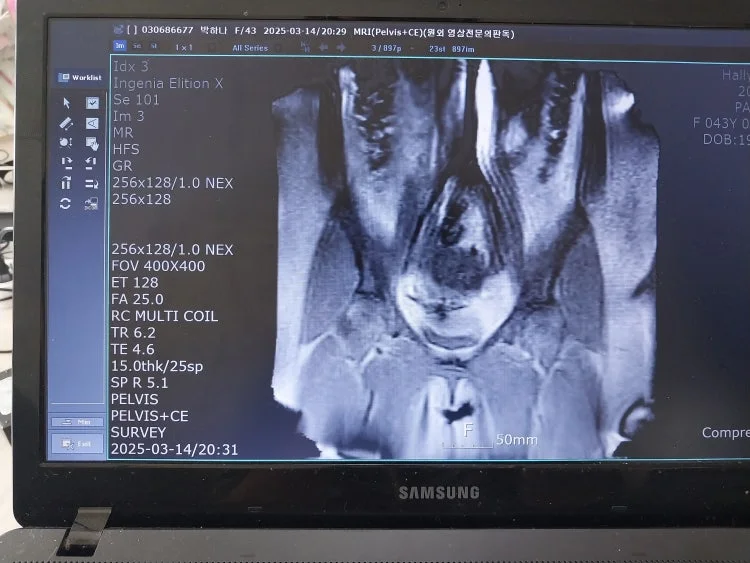
Please review my uterine MRI results.
Please review my uterine MRI results.
I was told by my doctor that I have adenomyosis.
However, the doctor’s explanation was confusing. They said it’s adenomyosis, but at the same time, they told me the results were “normal” and asked me if that’s what the MRI showed. Then they added that the diagnosis of adenomyosis is something they determine themselves — not solely based on MRI results.
So they said I do have adenomyosis, but also told me it’s nothing to worry about, which left me confused.
That’s why I’d like to ask for your help in understanding this.
On ultrasound, my uterus size appeared normal. A few days before the MRI, I received a hormone injection to induce menstruation. About 5–6 days after the MRI, my period started.
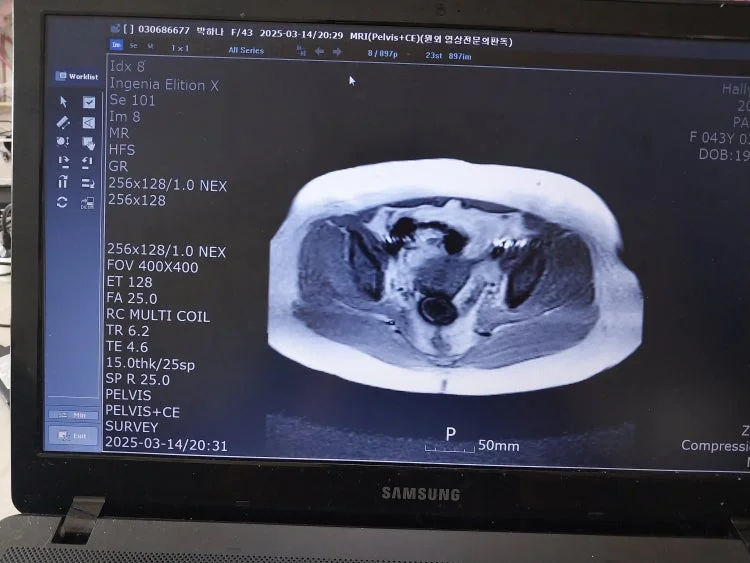
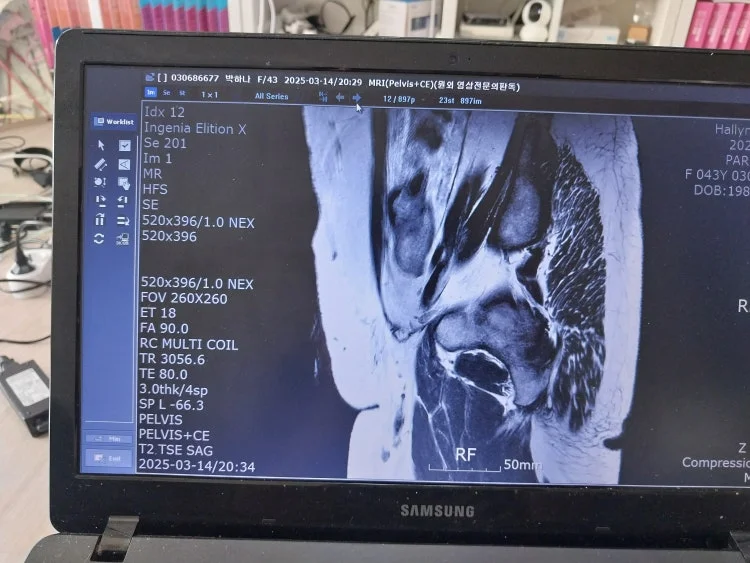
I was told that my uterus is enlarged — I’d like to know if that’s correct and, if so, how enlarged it is. I also want to know if I truly have adenomyosis based on these findings.
Here’s a brief medical history:
Around November, I experienced irregular bleeding for about two months. The doctor found thickened endometrium and recommended curettage and a biopsy.
I had the D&C (dilation and curettage) procedure on January 9th.
After that, I began having lower abdominal pain, pelvic pain, and lower back pain.
I visited several OB-GYN clinics; ultrasounds showed no abnormalities, and other doctors told me it wasn’t adenomyosis.
I didn’t have a period for two months, so I got a hormone shot on March 11th to induce menstruation.
The pain continued, so I had an MRI on March 14th.
My period started on March 20th, and the menstrual flow was very heavy for 3–4 days.
In the end, they told me the diagnosis was adenomyosis.
I would really appreciate it if you could help me understand the MRI results more clearly and explain whether adenomyosis is confirmed and how severe it might be.